Article highlights & insights
Cytotoxic therapies, such as chemotherapy and radiotherapy, constitute mainstays of cancer treatment for both early-stage cancer and unresectable advanced disease. In addition to inducing tumour shrinkage through direct cytotoxic effects on proliferating cancer cells, these therapies can also stimulate the immune system to help control tumour outgrowth. However, chemoresistance and tumour relapse continue to pose significant challenges, indicating that anti-cancer immunity following cytotoxic therapy may be weak, short-lived, or overridden by immune evasive mechanisms.
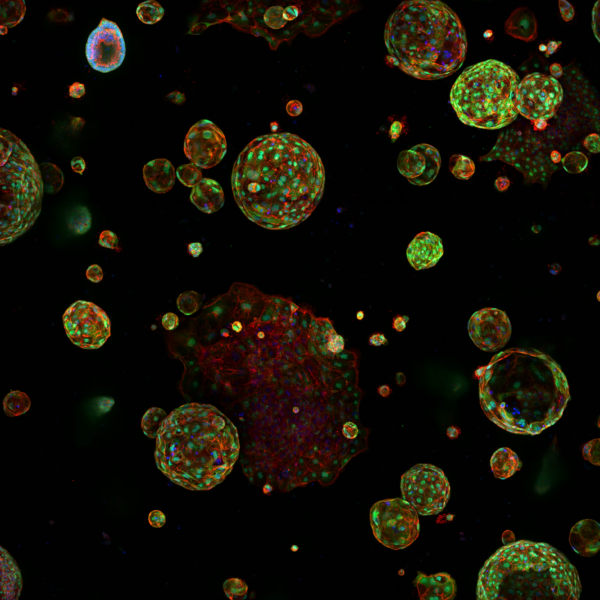
Previous studies have implicated prostaglandin E2 (PGE2) release from dying cancer cells in stimulating cancer cell proliferation and tumour repopulation postcytotoxic therapy. In this study, the Cancer Immunity and Inflammation group revealed that upregulation of the cyclooxygenase (COX)-2/PGE2 pathway in cancer cells after chemotherapy is a widespread phenomenon that alters the inflammatory properties of the treated dying cancer cells. By screening multiple mouse and human cancer lines, the group showed that enhanced PGE2 synthesis postcytotoxic treatment is an active process that occurs only when the cancer cells have pre-existing COX-2 expression and activity.
Using a library of >1200 market-approved compounds added to COX-2-transcription reporter cancer cells combined with quantitative real-time live-cell imaging, they found that all classes of anti-neoplastic drugs rapidly upregulated COX-2. This phenomenon coincided with the arrest of cancer cell proliferation induced by the various neoplastic agents independently of their mechanism of action.
These data indicate that the upregulation of COX-2/PGE2 by cancer cells undergoing cell death might be a significant obstacle to the development of tumour immunity resulting from cytotoxic therapy. Accordingly, tumour shrinkage and inhibition of metastatic spread using a poorly immunogenic breast cancer model was exclusively observed following the triple combination of PD-1 blockade, chemotherapy and a selective COX-2 inhibitor. Thus, this study highlights a potential approach for enhancing the effectiveness of combinations of immunotherapy and chemotherapy.
Cytotoxic therapies, such as chemotherapy and radiotherapy, constitute mainstays of cancer treatment for both early-stage cancer and unresectable advanced disease. In addition to inducing tumour shrinkage through direct cytotoxic effects on proliferating cancer cells, these therapies can also stimulate the immune system to help control tumour outgrowth. However, chemoresistance and tumour relapse continue to pose significant challenges, indicating that anti-cancer immunity following cytotoxic therapy may be weak, short-lived, or overridden by immune evasive mechanisms.
Previous studies have implicated prostaglandin E2 (PGE2) release from dying cancer cells in stimulating cancer cell proliferation and tumour repopulation postcytotoxic therapy. In this study, the Cancer Immunity and Inflammation group revealed that upregulation of the cyclooxygenase (COX)-2/PGE2 pathway in cancer cells after chemotherapy is a widespread phenomenon that alters the inflammatory properties of the treated dying cancer cells. By screening multiple mouse and human cancer lines, the group showed that enhanced PGE2 synthesis postcytotoxic treatment is an active process that occurs only when the cancer cells have pre-existing COX-2 expression and activity.
Using a library of >1200 market-approved compounds added to COX-2-transcription reporter cancer cells combined with quantitative real-time live-cell imaging, they found that all classes of anti-neoplastic drugs rapidly upregulated COX-2. This phenomenon coincided with the arrest of cancer cell proliferation induced by the various neoplastic agents independently of their mechanism of action.
These data indicate that the upregulation of COX-2/PGE2 by cancer cells undergoing cell death might be a significant obstacle to the development of tumour immunity resulting from cytotoxic therapy. Accordingly, tumour shrinkage and inhibition of metastatic spread using a poorly immunogenic breast cancer model was exclusively observed following the triple combination of PD-1 blockade, chemotherapy and a selective COX-2 inhibitor. Thus, this study highlights a potential approach for enhancing the effectiveness of combinations of immunotherapy and chemotherapy.