Article highlights & insights
Small cell lung cancer is a highly vascularised, aggressive neuroendocrine (NE) cancer associated with high mortality. SCLC treatment has remained unchanged in decades, with the recent introduction of immunotherapy benefiting a minority of unselected patients. There is increasing understanding of SCLC heterogeneity, including SCLC molecular subtypes based on expression of NE and non-NE transcription factors (TFs). Additionally, SCLC plasticity via NE to non-NE phenotype transition is linked with metastasis, chemoresistance, and immune evasion. Whilst personalised medicine approaches attempt to exploit molecular subtype differences, an incomplete understanding of the functional significance of NE to non-NE plasticity creates additional complexity.
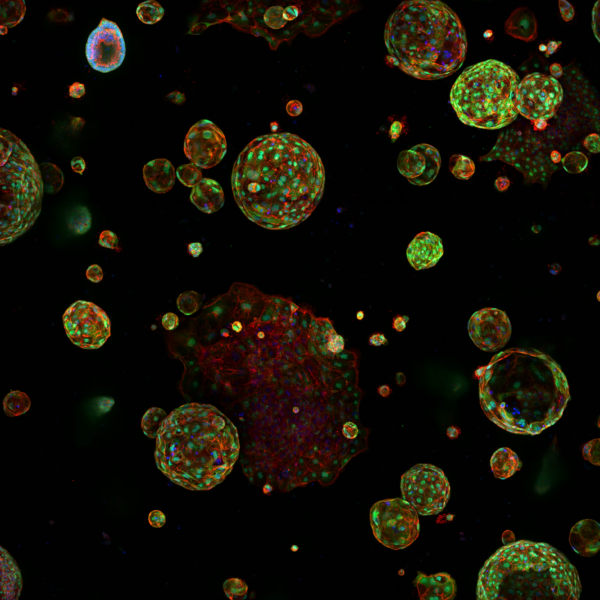
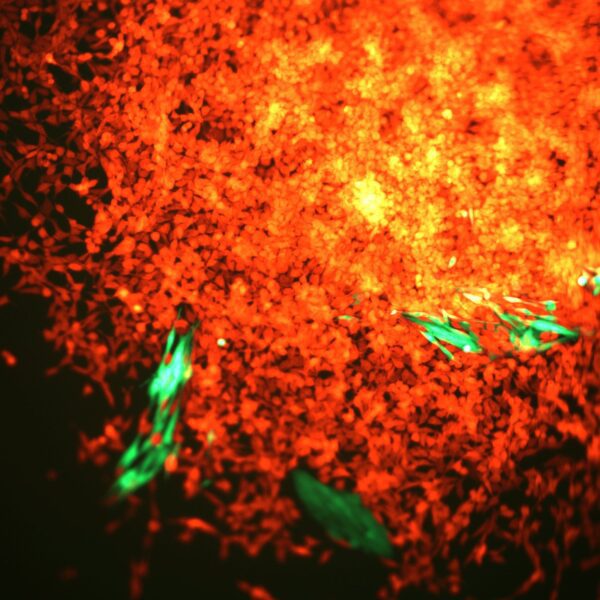
Using SCLC circulating tumour cell (CTC)-derived tumour explant (CDX) models, the authors report the first functional evidence of the role of NOTCH-driven NE to Non-NE plasticity in SCLC, facilitating vasculogenic mimicry (VM). VM is an angiogenesis-independent epithelial-to-endothelial transition of tumour cells to acquire endothelial properties and form de novo vessels. Immunohistochemistry showed co-localisation of VM vessels with the non-NE marker REST in vivo whilst ex vivo cultures of isolated non-NE and NE cell populations showed only non-NE cells could form hollow tubules on Matrigel (the gold-standard surrogate assay for VM competency). Moreover, intravenous injection of lectin to CDX-bearing mice revealed that VM vessels are functionally perfused in vivo.
RNAseq of NE and non-NE cell populations showed that non-NE cells are transcriptionally primed to undergo tubule formation and are enriched for hypoxic, vascular endothelial and ECM remodelling gene signatures, hinting at hypoxia being a putative VM driver. Ex vivo studies with different growth substrates, dye-quenched collagen and integrin blocking antibodies revealed that tubule formation by non-NE cells is regulated by β1-integrin-mediated collagen remodelling.
Overall, these data highlight the need to target both NE and non-NE cells to effectively inhibit VM and have prompted further studies to understand its role in supporting tumour growth and metastasis.
Small cell lung cancer is a highly vascularised, aggressive neuroendocrine (NE) cancer associated with high mortality. SCLC treatment has remained unchanged in decades, with the recent introduction of immunotherapy benefiting a minority of unselected patients. There is increasing understanding of SCLC heterogeneity, including SCLC molecular subtypes based on expression of NE and non-NE transcription factors (TFs). Additionally, SCLC plasticity via NE to non-NE phenotype transition is linked with metastasis, chemoresistance, and immune evasion. Whilst personalised medicine approaches attempt to exploit molecular subtype differences, an incomplete understanding of the functional significance of NE to non-NE plasticity creates additional complexity.
Using SCLC circulating tumour cell (CTC)-derived tumour explant (CDX) models, the authors report the first functional evidence of the role of NOTCH-driven NE to Non-NE plasticity in SCLC, facilitating vasculogenic mimicry (VM). VM is an angiogenesis-independent epithelial-to-endothelial transition of tumour cells to acquire endothelial properties and form de novo vessels. Immunohistochemistry showed co-localisation of VM vessels with the non-NE marker REST in vivo whilst ex vivo cultures of isolated non-NE and NE cell populations showed only non-NE cells could form hollow tubules on Matrigel (the gold-standard surrogate assay for VM competency). Moreover, intravenous injection of lectin to CDX-bearing mice revealed that VM vessels are functionally perfused in vivo.
RNAseq of NE and non-NE cell populations showed that non-NE cells are transcriptionally primed to undergo tubule formation and are enriched for hypoxic, vascular endothelial and ECM remodelling gene signatures, hinting at hypoxia being a putative VM driver. Ex vivo studies with different growth substrates, dye-quenched collagen and integrin blocking antibodies revealed that tubule formation by non-NE cells is regulated by β1-integrin-mediated collagen remodelling.
Overall, these data highlight the need to target both NE and non-NE cells to effectively inhibit VM and have prompted further studies to understand its role in supporting tumour growth and metastasis.
Institute Authors
Group leader
Research topics & keywords
Meet the Research Team
Here are the authors from the Small Cell Lung Cancer Biology group that contributed to this paper.
Our Research
Our research spans the whole spectrum of cancer research from cell biology through to translational and clinical studies
Research Groups
Our research groups study many fundamental questions of cancer biology and treatment
Our Facilities
The Institute has outstanding core facilities that offer cutting edge instruments and tailored services from expert staff
Latest News & Updates
Find out all our latest news
Careers that have a lasting impact on cancer research and patient care
We are always on the lookout for talented and motivated people to join us. Whether your background is in biological or chemical sciences, mathematics or finance, computer science or logistics, use the links below to see roles across the Institute in our core facilities, operations teams, research groups, and studentships within our exceptional graduate programme.